Book Appointment Now
Geriatric Diabetes Management: Evidence-Based Project
Geriatric Diabetes Management: Evidence-Based Project focuses on addressing the unique challenges of managing diabetes in older adults, a population increasingly affected by this chronic condition. Diabetes in elderly individuals is often complicated by comorbidities, frailty, polypharmacy, and age-related physiological changes, making evidence-based interventions critical. According to the Centers for Disease Control and Prevention (CDC, 2022), over 20% of individuals aged 65 and older in the United States live with diabetes, contributing to significant morbidity and healthcare costs. This paper explores the theoretical frameworks guiding geriatric diabetes care, examines the multifaceted impacts of the condition, and highlights the role of case managers in implementing evidence-based strategies to improve outcomes.
Get a custom paper help about geriatric diabetes management
Order Custom Nursing Paper
Theoretical Framework of Reference
Theoretical models such as the Orem’s Self-Care Deficit Nursing Theory and the Chronic Care Model (CCM) provide a solid foundation for geriatric diabetes management. The Self-Care Deficit Theory emphasizes that aging and chronic diseases, such as diabetes, can diminish an individual’s capacity for self-care, necessitating tailored interventions from healthcare providers (Orem, 2001). This framework highlights the importance of assessing patients’ abilities to adhere to diabetes management plans and addressing their specific deficits.
The Chronic Care Model, on the other hand, focuses on the integration of evidence-based practices, clinical expertise, and patient education to optimize chronic disease management (Wagner et al., 2001). It underscores the importance of team-based care and the use of decision-support tools in managing diabetes in older adults. Additionally, the Health Belief Model (HBM) provides insights into patient behavior, suggesting that elderly patients are more likely to adhere to diabetes management plans if they perceive the benefits of interventions and understand the risks of complications (Champion & Skinner, 2008). These frameworks collectively guide evidence-based projects aimed at improving outcomes in geriatric diabetes management.
Dimensions of Affected Individuals
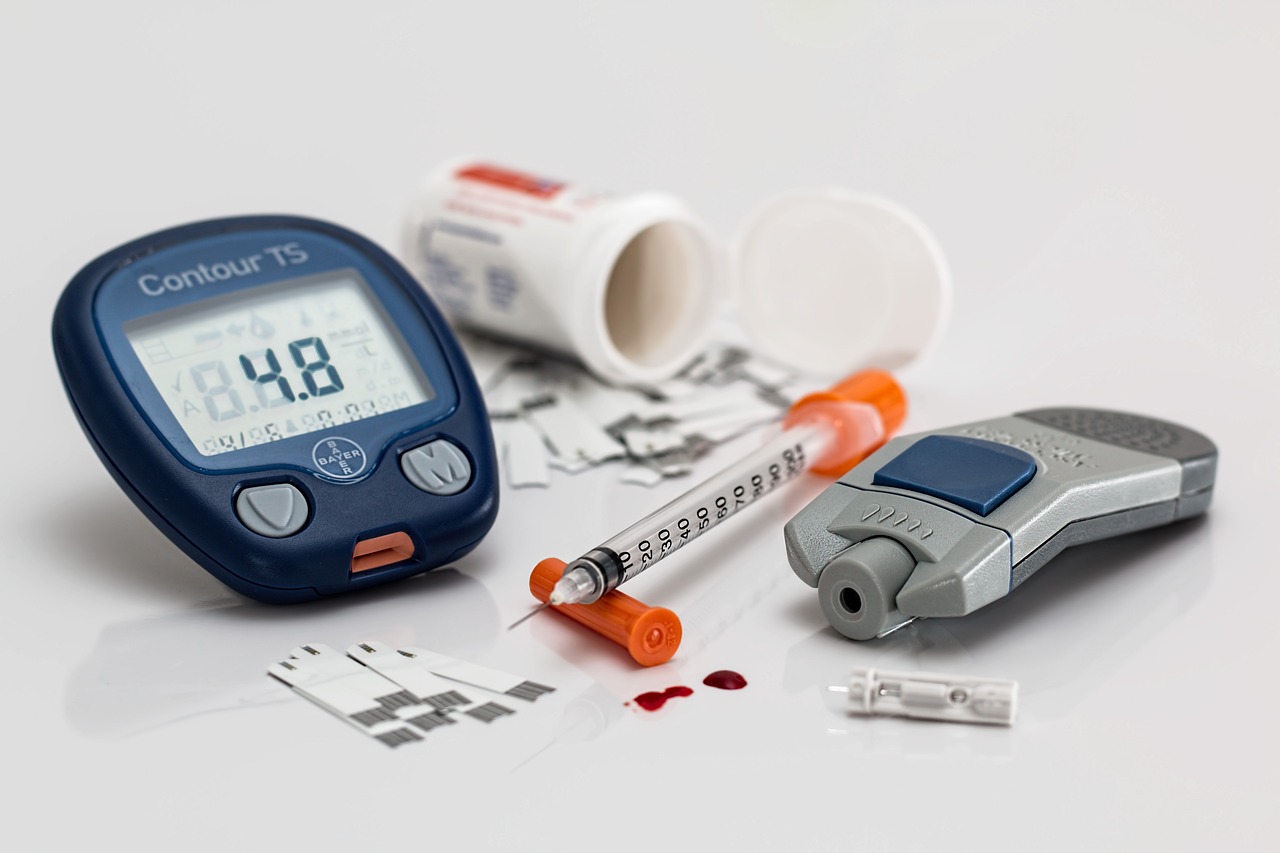
Diabetes significantly impacts the physical, emotional, and social dimensions of older adults. Physically, diabetes is associated with complications such as cardiovascular disease, neuropathy, nephropathy, and vision loss. Age-related frailty exacerbates these complications, making diabetes management more complex. Furthermore, hypoglycemia risk increases in the elderly due to altered drug metabolism and reduced renal function, necessitating careful monitoring of blood glucose levels (American Diabetes Association, 2022).
Emotionally, living with diabetes can lead to anxiety and depression, particularly in elderly patients facing functional limitations or reduced independence. Research highlights that 20-30% of older adults with diabetes experience symptoms of depression, which can negatively impact treatment adherence (Anderson et al., 2017). Socially, diabetes management often involves caregivers or family members, which can strain relationships and lead to feelings of dependency among patients. Cultural beliefs also play a role in shaping how older adults perceive and manage diabetes. For example, certain cultures may prioritize traditional remedies over medical interventions, which can influence adherence to evidence-based care plans.
Development of the Case Manager Role Using EBP
The role of the case manager is central to implementing evidence-based strategies for geriatric diabetes management. A case manager coordinates care across multidisciplinary teams, ensuring that the unique needs of elderly patients are addressed. One evidence-based strategy involves creating individualized care plans that account for comorbidities, functional status, and patient preferences. For instance, adjusting glycemic targets to avoid hypoglycemia in frail patients is an important consideration in older populations (ADA, 2022).
Another evidence-based approach involves integrating technology, such as continuous glucose monitoring systems and telemedicine, to improve patient self-monitoring and access to care. Studies show that these tools can enhance glycemic control and reduce hospital admissions (Li et al., 2020). Additionally, case managers play a pivotal role in patient education, ensuring that elderly individuals and their caregivers understand the importance of medication adherence, diet, and physical activity in managing diabetes. Advocacy for addressing social determinants of health, such as financial barriers to accessing insulin or glucose-monitoring devices, is also a critical component of the case manager’s role.
Conclusion
Geriatric Diabetes Management: Evidence-Based Project highlights the importance of tailored, evidence-based approaches to address the complexities of diabetes in older adults. By leveraging frameworks such as the Chronic Care Model and the Dorothea Orem Self-Care Deficit Nursing Theory, healthcare providers can develop personalized care plans that address the multifaceted impacts of diabetes. Case managers play a crucial role in coordinating care, implementing technological solutions, and advocating for patient-centered interventions. Ultimately, evidence-based strategies provide a pathway to improve glycemic control, reduce complications, and enhance the quality of life for older adults with diabetes.
Also read:
References
- American Diabetes Association (ADA). (2022). Standards of medical care in diabetes—2022. Diabetes Care, 45(Suppl 1), S1-S2.
- Anderson, R. J., et al. (2017). Prevalence of depression in adults with diabetes: A systematic review. Diabetes Care, 40(4), 529-534.
- Centers for Disease Control and Prevention (CDC). (2022). National diabetes statistics report. Retrieved from www.cdc.gov.
- Champion, V. L., & Skinner, C. S. (2008). The health belief model. Health behavior and health education: Theory, research, and practice, 45-65.
- Li, R., et al. (2020). Effectiveness of telemedicine interventions for diabetes management in older adults: A meta-analysis. Journal of Diabetes Science and Technology, 14(1), 24-33.
- Orem, D. E. (2001). Nursing: Concepts of practice (6th ed.). Mosby.
- Wagner, E. H., et al. (2001). Improving chronic illness care: Translating evidence into action. Health Affairs, 20(6), 64-78.