Book Appointment Now
Patient Portals in Evidence-Based Practice
Patient Portals in Evidence-Based Practice represent a transformative tool for enhancing patient engagement, improving adherence to treatment plans, and fostering better healthcare outcomes. These secure online platforms allow patients to access their medical records, communicate with healthcare providers, schedule appointments, and view treatment instructions anytime. Research has shown that patients who use portals are more likely to follow their prescribed care plans, leading to improved management of chronic conditions and higher satisfaction rates (Kruse et al., 2015). This paper explores the impact of patient portals in evidence-based practice, their multidimensional benefits, and the challenges associated with their implementation in clinical settings.
Get a custom paper help about the impact of patient portals in evidence-based practice
Order Custom Nursing Paper
Theoretical Framework of Reference
Patient portals align with several theoretical frameworks that underpin their application in evidence-based practice. The Health Belief Model (HBM) provides insights into how patient portals influence health behaviors. By giving patients access to detailed information about their conditions and treatments, portals enhance patients’ perceived benefits of adherence while reducing perceived barriers to accessing care (Champion & Skinner, 2008).
The Technology Acceptance Model (TAM) explains how ease of use and perceived usefulness drive patients’ adoption of patient portals. Ensuring that portals are user-friendly and clearly beneficial encourages widespread utilization among diverse populations (Davis, 1989).
Lastly, the Chronic Care Model (CCM) emphasizes the role of digital tools like patient portals in fostering self-management and improving coordination between patients and healthcare providers (Wagner et al., 2001). Together, these frameworks support the integration of patient portals into evidence-based healthcare delivery.
Dimensions of Patient Portals
The use of patient portals impacts several dimensions of healthcare, including physical health, emotional well-being, and the patient-provider relationship.
Physical Health: Patient portals support improved management of chronic conditions by facilitating access to medical records, test results, and tailored health recommendations. For example, diabetic patients can monitor their blood glucose trends, review dietary advice, and track medication adherence through portal features. A study found that portal use reduced HbA1c levels in patients with diabetes by promoting self-management (Turvey et al., 2014).
Emotional Well-Being: Patients who use portals report higher satisfaction and reduced anxiety about their health because they feel more informed and involved in their care. Features like secure messaging with providers offer reassurance and timely responses to health concerns, reducing stress and uncertainty.
Patient-Provider Relationship: Portals strengthen communication by providing a convenient platform for patients to ask questions, request medication refills, and receive follow-up instructions. This continuous engagement fosters trust and enhances the overall quality of care.
Evidence-Based Benefits of Patient Portals
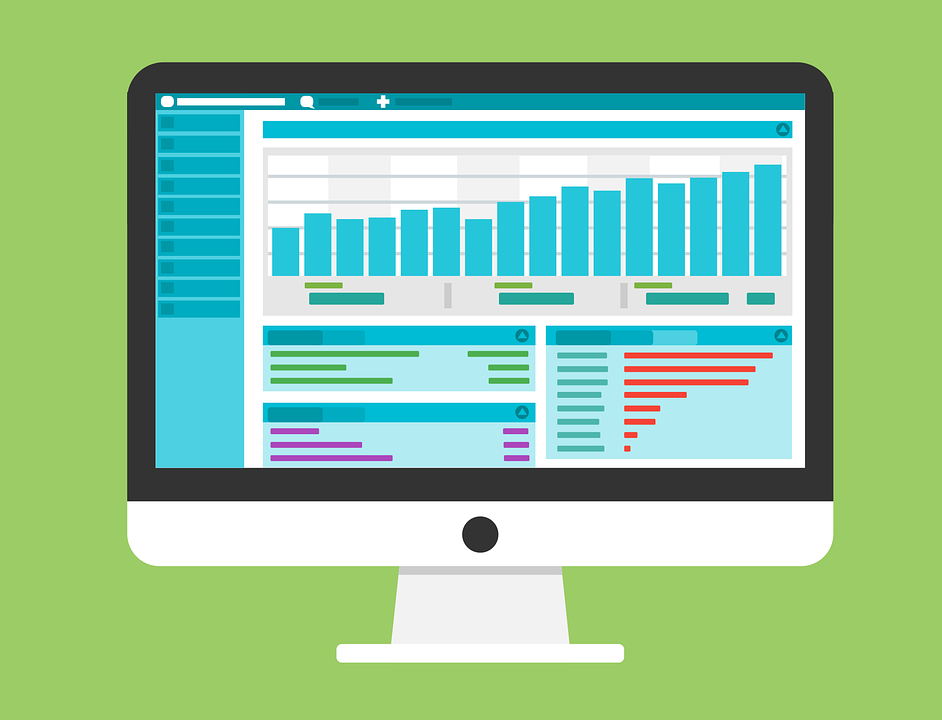
Patient portals have been shown to improve healthcare outcomes through increased patient engagement, enhanced adherence to treatment plans, and improved coordination of care.
Improved Patient Engagement: Evidence shows that patients who actively use portals are more engaged in their care. Features like appointment scheduling, prescription renewals, and preventive care reminders empower patients to take a proactive role in managing their health (Ammenwerth et al., 2012).
Enhanced Adherence: Portals improve adherence to treatment plans by making instructions easily accessible. For example, patients recovering from surgery can log in to view wound care instructions or reminders to take medications, reducing complications and readmissions.
Better Coordination of Care: Portals streamline communication between patients and healthcare teams, ensuring that critical information is readily available to all stakeholders. In multi-disciplinary care settings, patient portals facilitate the sharing of lab results, referrals, and care plans, improving continuity of care.
Health Outcomes: Studies have shown that portal use is associated with better health outcomes, including improved control of chronic conditions, reduced emergency room visits, and fewer hospitalizations (Krist et al., 2014).
Challenges in Implementing Patient Portals
Despite their benefits, patient portals face several challenges in implementation and utilization.
Digital Divide: Limited access to technology and the internet remains a significant barrier, particularly for elderly patients or those in low-income or rural areas. Addressing this issue requires investments in digital infrastructure and targeted education programs.
Health Literacy: Patients with low health literacy may struggle to understand medical terminology or navigate complex portal features. Simplifying the interface and providing tutorials or technical support can improve accessibility.
Privacy Concerns: Ensuring the security of patient data is critical to gaining trust in portal systems. Robust encryption protocols and compliance with regulations like HIPAA are essential for protecting sensitive health information.
Provider Workload: While portals improve communication, they may increase the workload for providers by adding to the volume of patient messages or requests. Healthcare organizations must establish clear guidelines and allocate resources to manage this demand effectively.
Strategies for Successful Implementation
To maximize the potential of patient portals, healthcare organizations should adopt strategies that promote their accessibility, usability, and integration into care delivery.
User-Friendly Design: Designing intuitive interfaces with clear navigation ensures that patients of all demographics can use the portal effectively. Features like large fonts, language options, and voice assistance improve usability for older adults and non-native speakers.
Patient Education: Providing training sessions, instructional videos, and step-by-step guides helps patients understand the portal’s features and benefits. Healthcare providers can also demonstrate portal usage during clinic visits.
Provider Training: Educating providers about the benefits of patient portals and equipping them with tools to manage portal interactions effectively can improve adoption rates and optimize workflows.
Feedback Mechanisms: Regularly gathering feedback from patients and providers helps identify areas for improvement, ensuring that portals continue to meet users’ needs.
Conclusion
Patient Portals in Evidence-Based Practice play a critical role in modern healthcare, enhancing patient engagement, adherence to treatment plans, and health outcomes. By leveraging frameworks like the Health Belief Model and the Chronic Care Model, healthcare organizations can integrate patient portals into care delivery effectively. Despite challenges such as the digital divide and privacy concerns, strategies like user-friendly design, education, and provider training ensure successful implementation. As digital healthcare continues to evolve, patient portals will remain a vital tool for improving communication, empowering patients, and delivering evidence-based care.
References
- Ammenwerth, E., et al. (2012). Effects of patient portals on patient care: A systematic review. Journal of Medical Internet Research, 14(2), e25.
- Champion, V. L., & Skinner, C. S. (2008). The health belief model. Health Behavior and Health Education: Theory, Research, and Practice, 45-65.
- Davis, F. D. (1989). Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Quarterly, 13(3), 319-340.
- Kruse, C. S., et al. (2015). Patient and provider attitudes toward the use of patient portals for the management of chronic disease: A systematic review. Journal of Medical Internet Research, 17(2), e40.
- Krist, A. H., et al. (2014). Patient use of secure messaging and patient portals: A systematic review. Annals of Family Medicine, 12(3), 263-272.
- Turvey, C., et al. (2014). Patient portals and patient engagement: A state of the science review. Journal of the American Medical Informatics Association, 21(1), e40-e46.
- Wagner, E. H., et al. (2001). Improving chronic illness care: Translating evidence into action. Health Affairs, 20(6), 64-78.