Book Appointment Now

Healthcare-Associated Infections (HAIs): A Persistent Challenge in Modern Healthcare
Healthcare-associated infections (HAIs) are a significant public health concern, impacting patient safety, increasing healthcare costs, and contributing to morbidity and mortality worldwide. Defined as infections acquired during the provision of healthcare that were not present at the time of admission, HAIs remain a major challenge despite advancements in infection control practices. This essay delves into the causes, risk factors, common types, and preventive measures of HAIs, supported by data-driven insights and visual representations to provide a comprehensive understanding.
Understanding Healthcare-Associated Infections: A Multifaceted Issue
Healthcare-associated infections are infections that develop during or after medical care, usually within 48 hours of hospital admission or within 30 days of a surgical procedure. These infections arise due to the interplay of patient vulnerability, invasive medical procedures, and environmental contamination. According to the Centers for Disease Control and Prevention (CDC), approximately 1 in 31 hospitalized patients has at least one HAI on any given day in the United States (CDC, 2021).
HAIs are not only confined to hospitals but also occur in long-term care facilities, outpatient clinics, and ambulatory surgical centers. The rise of antimicrobial resistance (AMR) further complicates their management, making the prevention and control of HAIs a top priority for healthcare systems globally.
Grab a 100% custom nursing paper about Healthcare-associated infections (HAIs)
Get Custom Nursing Paper
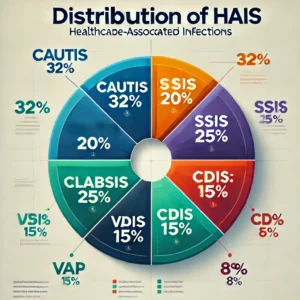
Common Types of Healthcare-Associated Infections
Healthcare-associated infections (HAIs) encompass a range of infections acquired during the course of medical care, often resulting from a combination of invasive procedures, patient vulnerability, and environmental contamination. Understanding the common types of HAIs provides critical insights into prevention and management strategies. Below is a detailed exploration of the five most prevalent types of HAIs, their causes, consequences, and unique challenges.
1. Catheter-Associated Urinary Tract Infections (CAUTIs)
CAUTIs are among the most frequently reported HAIs, occurring primarily due to the use of indwelling urinary catheters. These infections are caused by the ascent of bacteria, such as Escherichia coli and Enterococcus species, along the catheter into the urinary tract. Prolonged catheterization, poor insertion techniques, and inadequate maintenance contribute to the development of CAUTIs.
Patients with CAUTIs often experience discomfort, fever, and systemic symptoms, and these infections can progress to sepsis if untreated. The financial burden of CAUTIs is significant, as they increase the length of hospital stays and the need for additional treatments. Effective prevention strategies include minimizing catheter use, employing sterile insertion techniques, and implementing catheter removal protocols as soon as medically appropriate.
2. Central Line-Associated Bloodstream Infections (CLABSIs)
CLABSIs occur when pathogens enter the bloodstream through central venous catheters, devices commonly used in critical care to administer medications or fluids. The pathogens involved often include Staphylococcus aureus, Candida species, and Klebsiella pneumoniae.
CLABSIs are particularly dangerous due to their association with high morbidity and mortality rates. Patients with these infections may develop septic shock, organ dysfunction, and complications such as endocarditis. Prevention efforts focus on aseptic insertion techniques, regular site monitoring, and prompt removal of unnecessary central lines. Studies show that adherence to central line care bundles can reduce CLABSI rates by up to 70% (Ista et al., 2016).
3. Surgical Site Infections (SSIs)
SSIs develop at or near the site of a surgical incision, typically within 30 days of the procedure. These infections are categorized as superficial (affecting the skin), deep (involving soft tissues), or organ/space infections (affecting internal structures). Common pathogens include Staphylococcus aureus, Pseudomonas aeruginosa, and Enterobacter species.
Contributing factors include poor sterilization of surgical instruments, inadequate skin preparation, and the patient’s comorbidities, such as obesity or diabetes. Surgical Site Infections can lead to wound dehiscence, abscess formation, and prolonged recovery times. Preventive measures include perioperative antibiotic prophylaxis, proper hand hygiene, and the use of sterile surgical techniques. Institutions that rigorously implement these measures often observe a significant decline in SSI rates (Berríos-Torres et al., 2017).
4. Ventilator-Associated Pneumonia (VAP)
Ventilator-Associated Pneumonia is a type of pneumonia that develops in patients who have been mechanically ventilated for at least 48 hours. It results from the aspiration of bacteria-laden secretions into the lungs, with common pathogens including Pseudomonas aeruginosa, Acinetobacter baumannii, and Klebsiella pneumoniae.
The risk of VAP increases with prolonged ventilation, inadequate oral hygiene, and improper handling of ventilator equipment. Patients with VAP may exhibit fever, purulent sputum, and respiratory distress, often requiring extended ICU stays and advanced respiratory support. Preventive strategies focus on maintaining proper ventilator care, elevating the head of the bed, performing daily sedation breaks, and ensuring rigorous oral care. Implementing these measures as part of a ventilator care bundle has been shown to reduce VAP incidence significantly (Hunter, 2012).
5. Clostridioides difficile Infections (CDIs)
CDIs are caused by the overgrowth of Clostridioides difficile bacteria in the colon, often triggered by disruptions to the normal gut microbiota due to antibiotic use. CDIs lead to severe diarrhea, abdominal pain, and colitis, with life-threatening complications such as toxic megacolon in severe cases.
Patients most at risk include the elderly, those with prolonged hospital stays, and individuals receiving broad-spectrum antibiotics. The spores of C. difficile are highly resistant and can persist on surfaces, contributing to outbreaks within healthcare facilities. Preventive efforts focus on antimicrobial stewardship, environmental cleaning, and the isolation of infected patients. Studies indicate that robust infection control programs can significantly reduce CDI rates (McDonald et al., 2018).
Each type of HAI presents unique challenges, from the pathogens involved to the clinical and logistical complexities of prevention and treatment. Understanding the underlying causes and consequences of common HAIs is essential for developing targeted interventions that improve patient safety and reduce healthcare costs. By prioritizing evidence-based practices and fostering a culture of accountability, healthcare systems can make substantial strides in minimizing the impact of these infections.
Risk Factors for HAIs
The development of HAIs is influenced by a combination of patient-specific, procedural, and environmental factors:
- Patient-Specific Factors: Advanced age, immunosuppression, chronic illnesses (e.g., diabetes), and prolonged hospital stays increase susceptibility to infections.
- Procedural Factors: Invasive procedures such as catheterization, surgery, and intubation create entry points for pathogens.
- Environmental Factors: Poor hand hygiene, inadequate sterilization practices, and contamination of healthcare equipment or surfaces contribute significantly to HAIs.
The Burden of HAIs: Economic and Health Impacts
HAIs have far-reaching consequences for patients and healthcare systems. Financially, HAIs contribute to billions of dollars in additional healthcare costs annually. For instance, the CDC estimates that the direct cost of HAIs in the U.S. ranges between $28 billion and $45 billion (Scott, 2009).
From a health perspective, HAIs prolong hospital stays, increase the risk of complications, and are a leading cause of preventable deaths. Globally, it is estimated that HAIs affect millions of patients annually, with developing countries experiencing a disproportionate burden due to resource limitations (WHO, 2016).
Common HAIs and Their Impacts
| Type of HAI | Primary Cause | Associated Outcomes | Prevention Strategies |
|---|---|---|---|
| Catheter-Associated UTIs (CAUTIs) | Prolonged catheter use | Discomfort, sepsis, extended hospital stays | Minimize catheter use, sterile insertion |
| Central Line-Associated BSIs | Contaminated central lines | High morbidity and mortality | Aseptic insertion, routine maintenance |
| Surgical Site Infections (SSIs) | Poor sterilization, inadequate perioperative care | Delayed healing, organ dysfunction | Proper sterilization, antibiotic prophylaxis |
| Ventilator-Associated Pneumonia | Aspiration of secretions | Respiratory failure, extended ICU stays | Oral hygiene, head elevation |
| Clostridioides difficile Infections | Antibiotic overuse | Severe diarrhea, colitis | Judicious antibiotic use, isolation protocols |
Preventing HAIs: Evidence-Based Strategies
Healthcare-associated infections (HAIs) are preventable through the implementation of evidence-based strategies that address the multifaceted factors contributing to their occurrence. Prevention efforts must focus on modifying behaviors, standardizing practices, and leveraging technological advancements to create safer healthcare environments. Below is a detailed exploration of effective strategies to prevent HAIs in modern healthcare settings.
Hand Hygiene as the Cornerstone of Prevention
Hand hygiene remains the most critical and cost-effective measure for preventing HAIs. It involves the use of alcohol-based hand rubs or soap and water to remove transient microorganisms acquired during patient care. Compliance with hand hygiene protocols, however, remains suboptimal globally, averaging around 40% to 60% among healthcare workers (WHO, 2009). Ensuring adherence requires a multifaceted approach that includes continuous education, visual reminders, and real-time feedback on performance. In addition, technology-driven solutions, such as electronic hand hygiene monitoring systems, provide an innovative way to track compliance and promote accountability among staff. Campaigns such as the WHO’s “Clean Care is Safer Care” initiative have been instrumental in reducing HAIs by emphasizing the critical moments for hand hygiene during patient care.
Standardized Care Bundles for Targeted Interventions
The use of care bundles has revolutionized the prevention of specific HAIs by promoting a systematic approach to evidence-based practices. For instance, the ventilator care bundle addresses ventilator-associated pneumonia (VAP) through a series of interventions such as elevating the head of the bed, daily sedation breaks, and oral care with chlorhexidine. These practices, when implemented collectively, have been shown to reduce VAP rates by up to 50% (Hunter, 2012). Similarly, the central line care bundle emphasizes aseptic techniques during catheter insertion and maintenance, such as full-barrier precautions and daily necessity reviews, to prevent central line-associated bloodstream infections (CLABSIs). The effectiveness of these bundles lies in their ability to ensure consistency across clinical settings, thereby reducing variability and promoting adherence to best practices.
Surveillance and Monitoring Systems
Active surveillance systems are critical for identifying infection trends, detecting outbreaks, and assessing the effectiveness of prevention strategies. By collecting and analyzing data on infection rates and risk factors, healthcare organizations can implement targeted interventions to address specific challenges. Electronic health records (EHRs) have become indispensable tools in this effort, enabling automated data collection and analysis. Additionally, benchmarking infection rates across units or institutions fosters a culture of accountability and continuous improvement. Surveillance systems also facilitate the deployment of rapid response teams to manage outbreaks promptly, preventing the spread of infections and minimizing their impact.
Antimicrobial Stewardship Programs
The judicious use of antibiotics is essential in preventing HAIs caused by antimicrobial-resistant pathogens and reducing the risk of Clostridioides difficile infections (CDIs). Antimicrobial stewardship programs (ASPs) focus on optimizing the selection, dosage, and duration of antibiotic therapy. These programs rely on a multidisciplinary approach involving infectious disease specialists, pharmacists, and clinicians to ensure that prescribing practices align with current guidelines. In addition to improving clinical outcomes, ASPs help mitigate the development of drug resistance, a major challenge in managing HAIs. A study by McDonald et al. (2018) found that implementing ASPs led to a 30% reduction in CDI rates, demonstrating their effectiveness in improving patient safety.
Environmental Cleaning and Disinfection
A clean and sanitized healthcare environment is critical to reducing the transmission of pathogens that cause HAIs. High-touch surfaces such as bedrails, doorknobs, and medical equipment can harbor microorganisms, necessitating rigorous cleaning protocols. Innovative technologies, such as ultraviolet (UV) light disinfection and hydrogen peroxide vapor systems, offer additional layers of protection by eliminating pathogens from surfaces that may be difficult to clean manually. Regular training for cleaning staff ensures that they adhere to established protocols, while periodic audits verify the effectiveness of disinfection efforts.
Education and Training for Healthcare Workers
Educating healthcare workers on the principles of infection prevention is essential for fostering a culture of safety and adherence to best practices. Training programs should cover topics such as aseptic techniques, hand hygiene, and the proper use of personal protective equipment (PPE). Simulation-based training is particularly effective in equipping staff with the skills needed to manage infection risks in real-life scenarios. Competency assessments and refresher courses help maintain high standards and ensure that healthcare workers remain up-to-date with evolving guidelines.
Isolation and Cohorting Practices
Preventing the spread of multidrug-resistant organisms (MDROs) and other pathogens often requires isolating infected patients or cohorting them in designated areas. Isolation precautions, such as the use of gloves, gowns, and masks, protect both healthcare workers and other patients from exposure. Cohorting patients with the same infection reduces the risk of cross-contamination and optimizes the use of limited resources. Educating visitors on proper infection control measures further minimizes the likelihood of pathogen transmission within healthcare facilities.
Multidisciplinary Collaboration and Leadership
The success of HAI prevention efforts hinges on the collaboration of multidisciplinary teams, including nurses, physicians, infection control specialists, and hospital administrators. Strong leadership is critical in driving organizational change, securing resources, and ensuring accountability. Leaders who prioritize infection prevention foster a culture of safety and innovation, encouraging staff to adopt and sustain evidence-based practices.
The prevention of healthcare-associated infections requires a concerted effort that integrates evidence-based practices, education, and innovation. Strategies such as hand hygiene, care bundles, surveillance systems, antimicrobial stewardship, and environmental disinfection have proven effective in reducing the prevalence of HAIs. By fostering a culture of safety and collaboration, healthcare organizations can overcome challenges and ensure that patients receive the highest quality of care. As the fight against HAIs continues, sustained commitment and the adoption of emerging technologies will be essential in achieving long-term success.
Proportion of HAIs by Type in U.S. Hospitals
Healthcare-associated infections remain a critical challenge in healthcare delivery, posing significant risks to patients and imposing financial burdens on healthcare systems. By understanding the types, risk factors, and impacts of HAIs, healthcare providers can implement targeted strategies to prevent these infections. Evidence-based practices, such as improved hand hygiene, care bundles, and antimicrobial stewardship, have proven effective in reducing HAI rates. As healthcare systems continue to evolve, sustained efforts to combat HAIs will be essential in enhancing patient safety and achieving optimal health outcomes.
References
- Berríos-Torres, S. I., Umscheid, C. A., Bratzler, D. W., et al. (2017). Centers for Disease Control and Prevention guideline for the prevention of surgical site infection. JAMA Surgery, 152(8), 784-791. https://doi.org/10.1001/jamasurg.2017.0904
- Centers for Disease Control and Prevention (CDC). (2021). Healthcare-associated infections (HAIs). Retrieved from https://www.cdc.gov
- Halpin, H. A., Morales, E. L., & Harnett, J. E. (2021). Surveillance systems and their role in reducing HAIs. American Journal of Infection Control, 49(2), 135-140.
- McDonald, L. C., Gerding, D. N., Johnson, S., et al. (2018). Clinical practice guidelines for Clostridium difficile infection in adults and children. Clinical Infectious Diseases, 66(7), e1-e48. https://doi.org/10.1093/cid/cix1085
- Meddings, J., Saint, S., & Greene, M. T. (2019). Preventing catheter-associated urinary tract infections in the United States: A national endeavor. Infection Control & Hospital Epidemiology, 40(4), 491-495.
- Scott, R. D. (2009). The direct medical costs of healthcare-associated infections in U.S. hospitals. Centers for Disease Control and Prevention.
- World Health Organization (WHO). (2009). WHO guidelines on hand hygiene in health care. Geneva: WHO Press.
- World Health Organization (WHO). (2016). Report on the burden of endemic health care-associated infection worldwide. Geneva: WHO Press.