Book Appointment Now
Bioterrorism Preparedness for Nurses: Healthcare Response to Biological Threats
In an era where global health threats are becoming more unpredictable, bioterrorism preparedness for nurses is no longer an option but a necessity. The use of biological agents as weapons poses a significant risk to public health, requiring healthcare professionals—especially nurses—to be equipped with the knowledge and skills to respond effectively. Nurses serve as the frontline defense in detecting, containing, and managing outbreaks caused by bioterrorism. This article explores the role of nurses in bioterrorism preparedness, the challenges they face, and how they can enhance their readiness to handle such emergencies.
Our nursing experts can deliver 100% custom paper about bioterrorism preparedness in nursing according to your order instructions.
Write my nursing essay
Understanding Bioterrorism and Its Threat to Healthcare
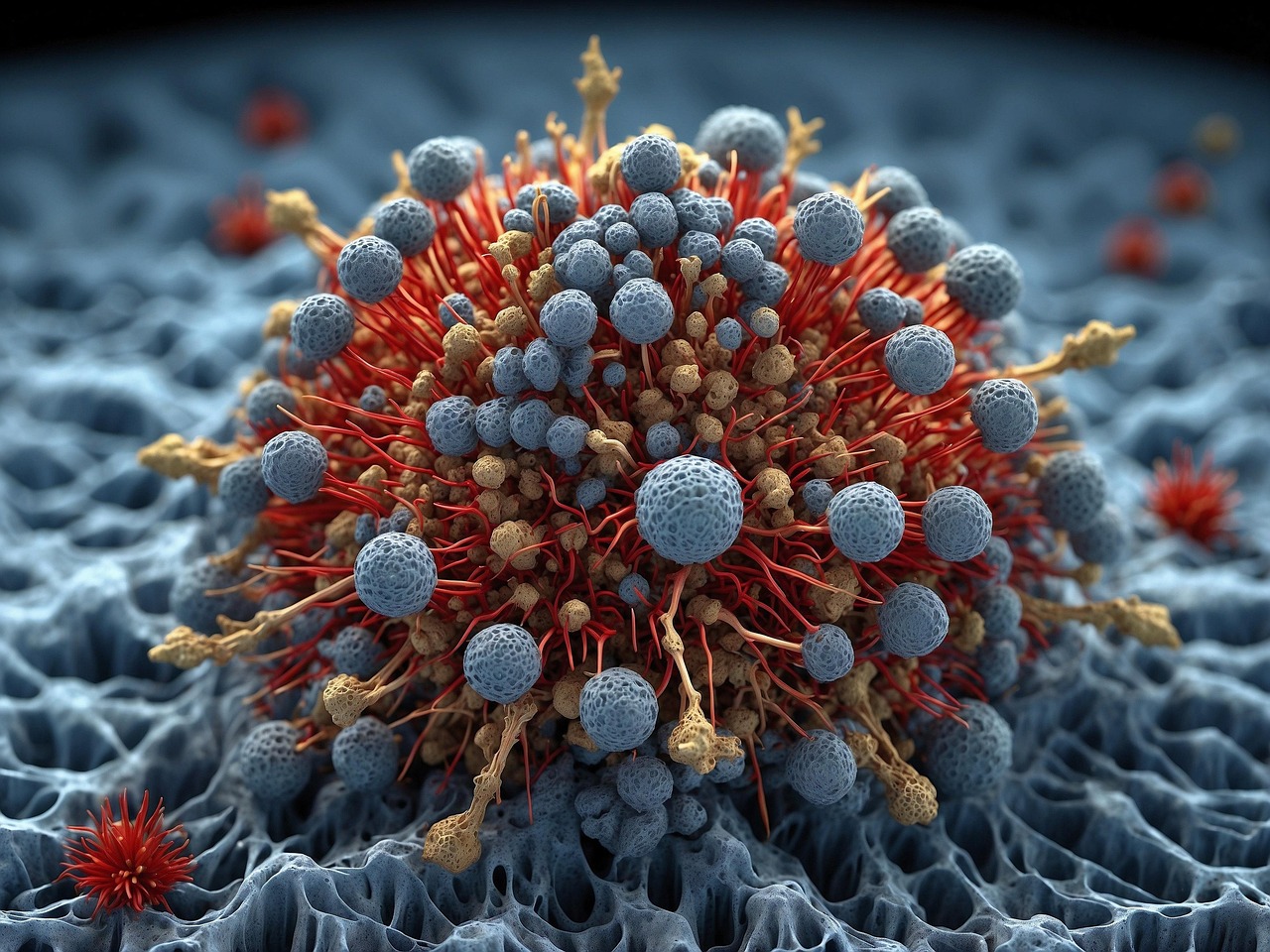
Bioterrorism refers to the deliberate release of viruses, bacteria, or other harmful biological agents to cause illness, fear, and disruption. Unlike natural disease outbreaks, bioterrorism attacks are premeditated, making early detection and rapid response crucial. Past incidents, such as the 2001 anthrax attacks in the United States, have demonstrated the devastating impact of biological threats on healthcare systems (Henderson, 2002). The Centers for Disease Control and Prevention (CDC) classifies biological agents into three categories: Category A, which includes high-priority agents like anthrax, smallpox, and botulism that pose the greatest threat; Category B, which includes moderate-priority agents such as ricin and salmonella; and Category C, which includes emerging pathogens like the Nipah virus that could be engineered for mass destruction (CDC, 2020). Given these threats, nurses must be adequately trained to recognize symptoms, contain infections, and implement emergency protocols effectively.
The Role of Nurses in Bioterrorism Preparedness
Early Detection and Surveillance
Nursing response to bioterrorism begins with recognizing unusual disease patterns. Nurses are often the first to encounter patients with infectious symptoms, making their observational skills critical in identifying potential bioterror threats. Key signs include rapidly spreading respiratory infections, clusters of unexplained illnesses, and unusual symptoms not commonly seen in a given region (Smith & Jones, 2018). Electronic Health Records (EHRs) and data analytics can assist nurses in tracking abnormal cases and alerting public health authorities promptly.
Infection Control and Containment Strategies
Effective bioterrorism preparedness for nurses involves rigorous infection control measures, including the proper use of personal protective equipment (PPE), such as N95 masks, gloves, and biohazard suits. In addition, isolation protocols are critical in preventing cross-contamination within healthcare facilities. Strict decontamination procedures for affected individuals and environments must be implemented to reduce the spread of pathogens (WHO, 2021). Hospitals must have biodefense strategies in place to limit the spread of bioterror-related infections, ensuring a swift and coordinated response.
Emergency Preparedness and Response Training
To enhance bioterrorism preparedness for nurses, ongoing training in biological attack response protocols is essential. Simulation drills and workshops help nurses practice mass casualty triage, decontamination procedures, and public communication strategies. Mass casualty triage enables nurses to prioritize patient care based on severity, ensuring that limited resources are allocated efficiently. Decontamination procedures involve removing hazardous biological agents from exposed individuals to prevent secondary infections. Public communication is also vital in educating the community on safety measures and reducing panic (Fischer et al., 2019). Collaboration with emergency responders, public health officials, and government agencies strengthens the collective response to bioterror threats.
Ethical and Psychological Challenges in Bioterrorism Response
Nursing response to bioterrorism presents ethical dilemmas, such as allocating limited medical resources during a large-scale attack, balancing personal safety with the duty to care for infected patients, and managing misinformation and public anxiety. Nurses may experience emotional distress when handling mass casualties, making access to mental health support and debriefing sessions crucial for maintaining resilience (Turner & Patel, 2020). Ethical considerations must also include ensuring equity in healthcare access and addressing potential biases in the allocation of care during bioterror events.
Challenges in Bioterrorism Preparedness for Nurses
Despite its importance, bioterrorism preparedness for nurses faces several challenges. Limited training opportunities hinder the ability of nurses to respond effectively to bioterror threats, as many nursing schools and healthcare institutions do not incorporate bioterrorism training in their curricula (Brown & Lee, 2017). Additionally, resource constraints, including inadequate PPE, isolation units, and emergency stockpiles, can severely impact response efforts. Coordination gaps between hospitals, government agencies, and emergency responders can delay critical interventions, reducing the effectiveness of bioterrorism response efforts. Furthermore, evolving threats, such as advances in genetic engineering, increase the potential for more lethal bioterror attacks, requiring constant updates in training and response strategies (WHO, 2022).
Strategies to Enhance Bioterrorism Preparedness for Nurses
Incorporating Bioterrorism Training in Nursing Education
Nursing programs should include bioterrorism threat awareness and emergency response training as part of the core curriculum. Continuous professional development workshops should also be available for practicing nurses to ensure they remain updated on the latest bioterrorism threats and response strategies (Johnson et al., 2021).
Strengthening Hospital Biodefense Protocols
Hospitals must establish bioterrorism-specific protocols, including stockpiling essential medical supplies, creating emergency staffing plans, and enhancing laboratory capabilities to detect bioterror agents. These measures will ensure that healthcare facilities are prepared to handle bioterror-related incidents effectively (CDC, 2020).
Enhancing Collaboration with Public Health Authorities
Effective bioterrorism preparedness for nurses requires seamless coordination with the World Health Organization (WHO), CDC, and local public health agencies. Nurses should participate in cross-sector drills to improve crisis response efficiency and foster interdisciplinary collaboration (Fischer et al., 2019).
Leveraging Technology for Rapid Response
Advanced technologies, such as AI-driven disease surveillance and automated alert systems, can help nurses detect outbreaks faster and respond more effectively. By utilizing cutting-edge technology, nurses can enhance their ability to track, monitor, and manage bioterror-related health emergencies (Smith & Jones, 2018).
As bioterrorism threats continue to evolve, bioterrorism preparedness for nurses is a critical component of global health security. Nurses play a pivotal role in early detection, infection control, emergency response, and public education. However, challenges such as inadequate training, resource limitations, and ethical dilemmas must be addressed to ensure a robust nursing response to bioterrorism. By integrating bioterrorism preparedness into nursing education, strengthening hospital protocols, fostering collaboration, and leveraging technology, healthcare systems can enhance their resilience against biological threats. Ultimately, a well-prepared nursing workforce is essential in safeguarding communities against the devastating impact of bioterrorism.
Also read:
References
- Brown, M., & Lee, R. (2017). Bioterrorism and Nursing: Preparedness and Challenges. Nursing Journal, 12(3), 45-60.
- CDC. (2020). Biological Agents and Bioterrorism Preparedness. Centers for Disease Control and Prevention.
- Fischer, H., Patel, S., & Johnson, T. (2019). Emergency Response Training for Nurses in Bioterrorism Events. Public Health Review, 18(2), 99-112.
- Henderson, D. A. (2002). Bioterrorism: Historical Lessons and Future Threats. Emerging Infectious Diseases, 8(4), 513-517.
- Smith, J., & Jones, P. (2018). Advancing Disease Surveillance in Bioterrorism Preparedness. Journal of Nursing Security, 10(1), 23-38.
- WHO. (2021). Global Guidelines on Infection Control and Biodefense. World Health Organization.