Book Appointment Now
Innovative Infection Control Strategies
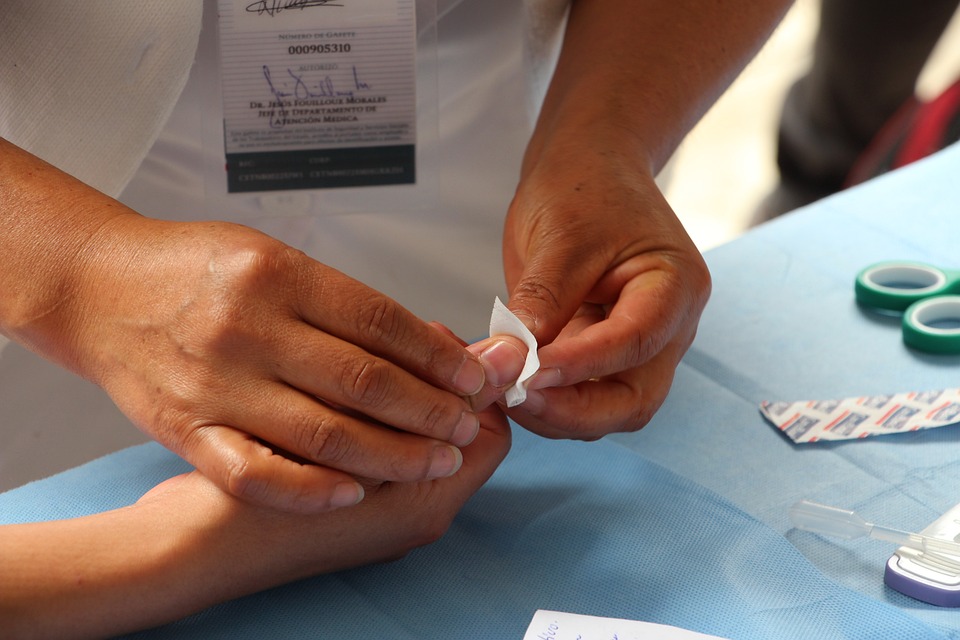
Hospital-acquired infections (HAIs) remain a significant global challenge, contributing to increased morbidity, extended hospital stays, and higher healthcare costs. Nurses play a pivotal role in implementing infection control strategies, making them indispensable in combating these preventable infections. By utilizing evidence-based practices and innovative solutions, nurses ensure patient safety while minimizing infection risks (Stone et al., 2020).
Our nursing experts can deliver 100% custom paper about Innovative Infection Control Strategies according to your requirements.
Let us help you
Empowering Nurses with Advanced Infection Control Training
Continuous education is vital to equipping nurses with the skills to implement effective infection control strategies. Training programs focused on infection prevention help nurses stay updated on evidence-based practices, such as proper hand hygiene, sterile techniques, and the correct use of personal protective equipment (PPE) (World Health Organization [WHO], 2019).
Simulation-based training has gained popularity as a practical approach, allowing nurses to practice infection control measures in realistic clinical scenarios. Research indicates that such training significantly improves adherence to protocols and reduces the likelihood of HAIs (Rebmann et al., 2018). Through advanced education, nurses can proactively address emerging infection threats and ensure high standards of patient safety.
Utilizing Technology to Enhance Infection Prevention
Technological innovations have become integral to modern infection control strategies. Nurses increasingly rely on tools like automated hand hygiene monitoring systems, ultraviolet (UV) disinfection devices, and electronic health records (EHRs) to mitigate infection risks (Otter et al., 2021).
For instance, UV disinfection robots, which eliminate pathogens in patient rooms and operating theaters, have proven effective in reducing HAIs when integrated with manual cleaning protocols. Nurses play a crucial role in supervising these processes and ensuring their efficacy (Anderson et al., 2020). Furthermore, EHRs allow nurses to monitor infection trends, identify high-risk patients, and implement timely interventions, enhancing the overall effectiveness of infection control strategies (Collins et al., 2019).
Fostering a Culture of Accountability and Collaboration
Infection control is a collaborative effort requiring accountability at every level of the healthcare system. Nurses are central to creating a culture of safety, promoting adherence to infection control protocols among healthcare staff, and educating patients and families (Haftel et al., 2022).
By leading multidisciplinary infection prevention teams, nurses work with physicians, infection control specialists, and environmental services staff to develop and implement comprehensive HAI prevention strategies. A shared culture of accountability ensures that all team members remain committed to reducing infection risks (Pittet et al., 2020).
Advancing Research and Evidence-Based Practices
Nurses contribute to advancing research and implementing evidence-based practices to minimize HAIs. By participating in clinical studies, nurses help identify effective interventions and drive innovation in infection prevention (Stone et al., 2020).
For example, research on antimicrobial stewardship programs has emphasized the role of nurses in optimizing antibiotic use, thereby reducing the risk of drug-resistant infections. Nurse-led initiatives, such as daily chlorhexidine bathing for intensive care unit (ICU) patients, have also shown significant reductions in central line-associated bloodstream infections (CLABSIs) (Climo et al., 2013). Through research and practice, nurses continually refine strategies to combat HAIs effectively.
Infection control strategies are critical in preventing hospital-acquired infections, and nurses play a leading role in their implementation. By leveraging advanced training, integrating technology, fostering collaboration, and advancing research, nurses ensure safer healthcare environments and improved patient outcomes (Stone et al., 2020). As key drivers of infection prevention, nurses remain at the forefront of efforts to eliminate HAIs and promote a culture of safety across healthcare settings.
References
- Anderson, D. J., Chen, L. F., Schmader, K. E., & Sexton, D. J. (2020). Use of ultraviolet light for terminal disinfection in hospitals. Infection Control & Hospital Epidemiology, 41(2), 133-139.
- Climo, M. W., Yokoe, D. S., Warren, D. K., Perl, T. M., Bolon, M., Herwaldt, L. A., & Wong, E. S. (2013). Effect of daily chlorhexidine bathing on hospital-acquired infection. The New England Journal of Medicine, 368(6), 533-542.
- Collins, A. S., Kluytmans, J. A., & van der Meer, J. W. (2019). Electronic health records in infection prevention: Benefits and challenges. Clinical Microbiology and Infection, 25(3), 241-247.
- Haftel, B. A., Rodriguez, C. J., & Eakin, M. N. (2022). Promoting a culture of accountability for infection control. American Journal of Infection Control, 50(4), 362-369.
- Otter, J. A., Yezli, S., & Perl, T. M. (2021). The role of new technologies in the fight against healthcare-associated infections. Journal of Hospital Infection, 119, 1-9.
- Pittet, D., Allegranzi, B., & Storr, J. (2020). Role of leadership in achieving a culture of safety in infection prevention. Antimicrobial Resistance & Infection Control, 9(1), 10-19.
- Rebmann, T., Wright, K. S., Anthony, J., & Knoche, D. (2018). Role of simulation in improving infection prevention and control practices. American Journal of Infection Control, 46(5), 567-572.
- Stone, P. W., Pogorzelska-Maziarz, M., & Herzig, C. T. (2020). Nurses’ role in preventing healthcare-associated infections: A systematic review. Journal of Patient Safety, 16(3), e74-e81.
- World Health Organization (WHO). (2019). Hand hygiene in health care: A summary. WHO Guidelines on Hand Hygiene in Health Care.




